Brain imaging (neuroimaging)
Brain imaging (neuroimaging)
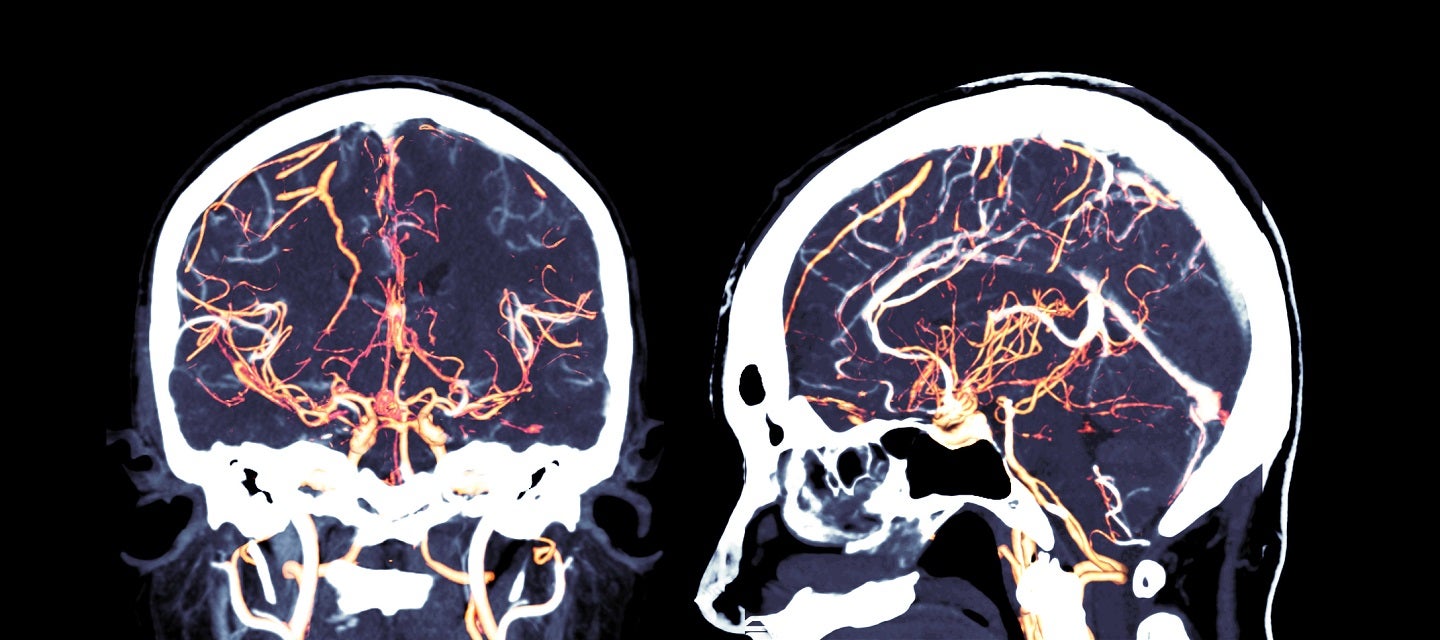
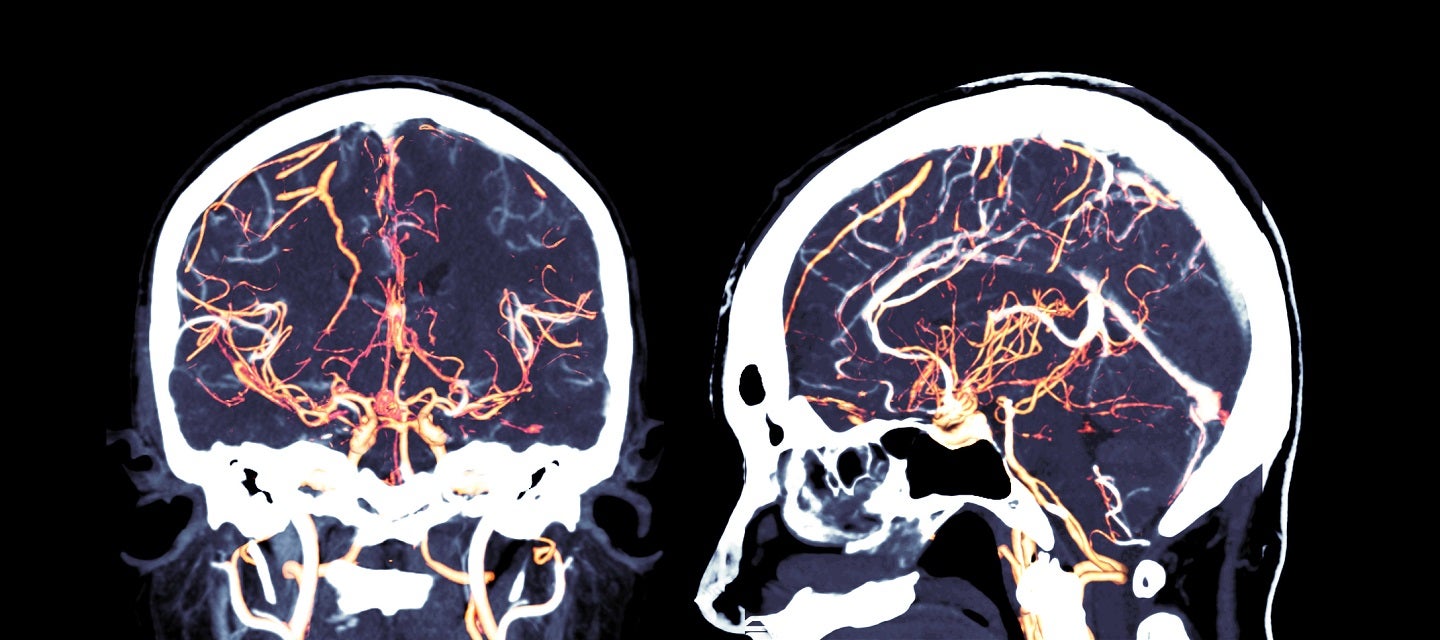
Focussing on the brain, neuroimaging is a branch of medical imaging that diagnoses disease and assesses brain health. Radiologists who specialise in the performance and interpretation of neuroimaging are known as neuroradiologists.
Structural imaging of the brain deals with the structure of the brain and the diagnosis of large-scale intracranial disease (such as a tumor), as well as injury.
Functional imaging of the brain is used to diagnose metabolic diseases and lesions on a finer scale (such as Alzheimer’s disease), and also for neurological and cognitive-psychology research. The brain’s information processing can be visualized directly when the involved area of the brain increases metabolism and “lights up” on the scan.
The brain in focus - webinar with neuroradiologist Dr Lynette Masters
Unexplained seizure in patients 16 years and over
Dr Ian Cox MBBS MMed FRANZCR is an experienced general radiologist with a special interest in MRI, neuroradiology and musculoskeletal imaging. Dr Cox is Director of MRI at I-MED Radiology Cabrini, a post he has held for more than 20 years. Here he presents some case studies to demonstrate when MRI is the preferred modality. Read more
Unexplained chronic headache
Headache is one of the most common medical symptoms. Although the majority of headache disorders are benign, it is a crucial (and challenging) task to decipher the benign variants from conditions that threaten life and neurological function. Usually a clinical history and examination is sufficient to diagnose a primary headache disorder, but when there is clinical doubt, investigations are required to exclude serious and treatable causes.
Deciding who needs investigation truly draws on a combination of the “science and art of medicine”. There are no easy answers, but there are a number of “red flags” that increase the chances of a serious underlying cause. These include a new onset or new type or worsening pattern of existing headache, new level of pain (e.g. “worst ever), headache triggered by valsalva or cough, by exertion, by sexual activity (pre-orgasmic, orgasmic), headache during pregnancy and puerperium (venous sinus thrombosis), headache where there are associated neurological signs or symptoms, or evidence of systemic illness including features of sepsis, immunosuppression, weight loss and cancer. New onset side-locked headache can be a symptom of arterial dissection, and postural headache is a symptom of spontaneous intracranial hypotension.
MRI is used to assess both the structure and the function of the central and peripheral nervous system, spine, and head and neck.
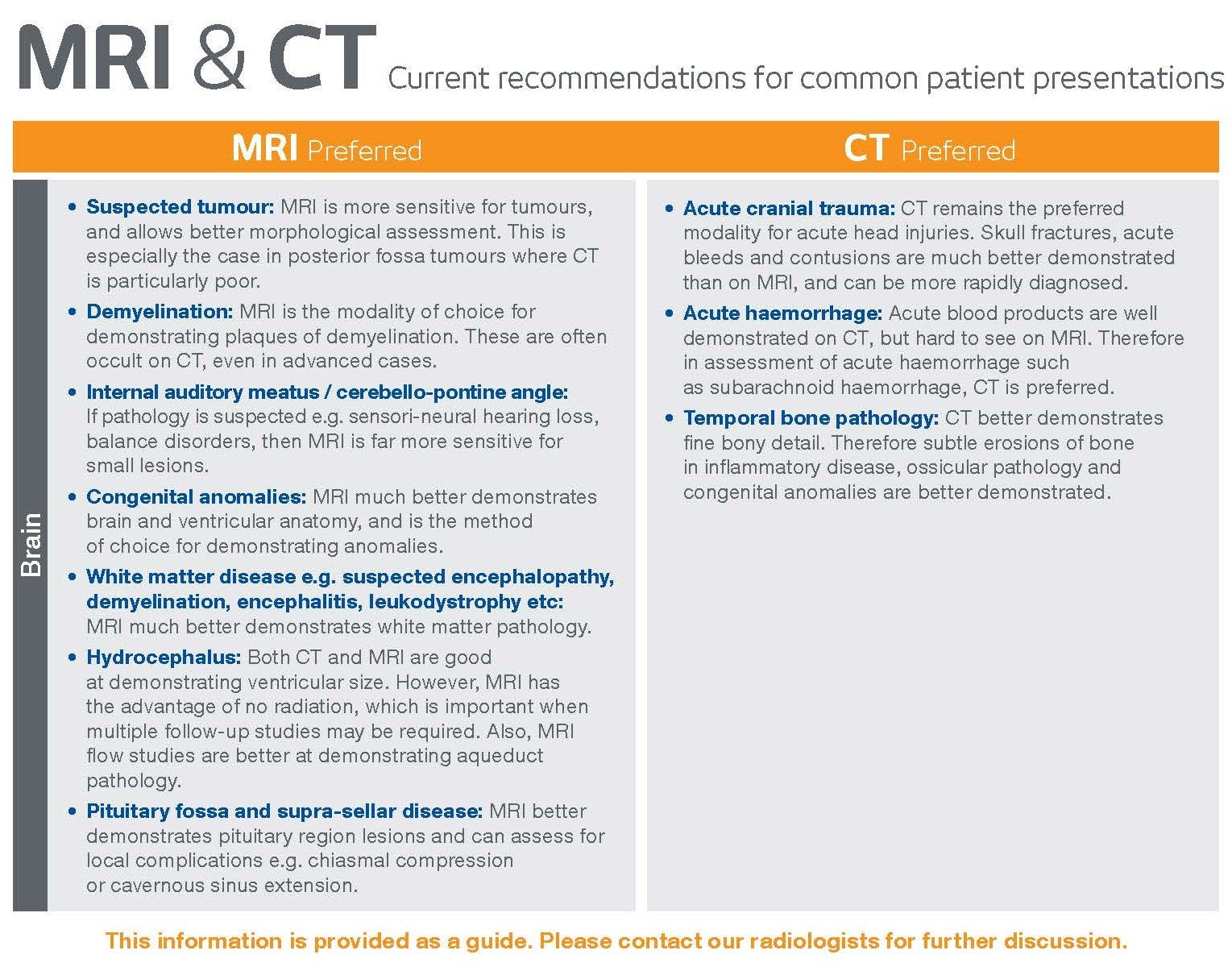
CT or MRI?
MRI is superior to CT for diagnosing most of the serious causes of chronic headache. CT remains the investigation of choice in headache associated with recent trauma, and in “thunder clap” headache that raises the possibility of subarachnoid haemorrhage.
CT and MRI are comparable in accuracy for diagnosing arterial dissection and venous sinus thrombosis, although dedicated CT angiography and venography (respectively) are necessary to make each diagnosis, and other causes of headache can easily be missed with these techniques
A “routine” MRI will detect a large number of causes of headache, and the sensitivity of MRI can be improved further by tailoring the examination to the patient. For this reason, it is even more important for MRI than CT that the request form contains the key clinical information. This is viewed by the radiologist before the MRI scan is performed, and the study is protocolled accordingly.
As MRI does not involve ionising radiation, and most patients with headache do not require IV contrast, investigation for headache is a safe, non-invasive process. Whilst many scans performed for headache will return a normal finding, the cost benefit comes from the reassurance to the patient and their doctor when the study is normal, and the vital benefit of detecting those patients with a serious, treatable condition before serious complications (including death) have occurred.
GP indications for MRI
GPs have access to some MRI rebates for conditions which commonly present in general practice, to help determine whether specialist referral is required, and/or to accelerate the patient management.
