
Your comprehensive breast care toolkit
Your comprehensive breast care toolkit

Key points
- This toolkit is designed to support women requiring supplementary screening or diagnostic breast imaging.
- The toolkit explains different types of breast screening, including screening and diagnostic mammography.
- Key breast health statistics highlight the prevalence of breast cancer and strong survival rates in Australia.
Breast care toolkit
Having the right knowledge empowers you to take control of your health. This toolkit enhances your understanding of breast health, screenings, and proactive wellness strategies. From differentiating between screening and diagnostic mammograms to mastering effective self-check techniques and understanding risk factors and symptoms, our resources are designed to to support women requiring supplementary screening or diagnostic breast imaging and guide on your breast care journey.
At the core of this toolkit is the belief that informed decisions lead to better outcomes. By gaining a deeper understanding of breast health, you can advocate for yourself with confidence and clarity.
Breast cancer in Australia
Breast cancer affects individuals and families both physically and emotionally. For those diagnosed, the journey involves surgeries, treatments, and emotional stress. Families often face financial challenges while providing care and support.

National Breast Cancer Foundation 2025.
Find more information on the Breast Cancer Trials website here.
Breast screening in Australia
BreastScreen Australia is the national Australian breast screening program and actively invites women aged 50–74 to have a free mammogram every two years. Women aged 40–49 and those aged over 74 are also eligible to receive a free mammogram, but do not receive an invitation and are advised to discuss the benefits with their doctor. High-risk women (eg, family history, BRCA gene mutation) of any age may require annual mammography and/or MRI and should consult with a GP or specialist for a personalised screening plan. Services are delivered through BreastScreen clinics located in hospitals, community health centres, and mobile vans (especially for regional/rural access).
Patients can use this calculator to calculate their risk: iPrevent - Peter MacCallum Cancer Centre
Private radiology providers also offer mammography (often with 3D tomosynthesis and same-day reporting), but these may attract an out-of-pocket cost.
BreastScreen vs diagnostic mammography – what is the difference?
Hear from an experienced I-MED Radiology mammographer who highlights the key difference between breast screening and diagnostic mammography, arming you with insights in the battle against breast cancer.
Diagnosing breast cancer keyboard_arrow_down
Mammography
A mammogram is a high-resolution x-ray used to identify breast changes that are suggestive of cancer or may be associated with increased risk of developing breast cancer. Mammograms are non-invasive and can be completed in around 20 minutes.
The latest technology is 3D mammography (known as tomosynthesis). It is beneficial in the detection of small breast cancers compared with conventional mammography, particularly in women with dense breast tissue, which can mask abnormal areas in a conventional mammogram. In some centers, intravenous contrast may be administered as part of the mammogram examination.
Ultrasound
A breast ultrasound will often follow a mammography study. It uses high frequency sound waves to produce an image of the tissues within the breast. The combination of the two examinations gives doctors more information, especially in younger patients.
Breast MRI
Breast MRI uses a magnetic field to take a series of images of the breast tissue. It does not use the ionising radiation of X-rays like a mammogram. It will usually involve an injection of a contrast agent into a vein in the arm during the scan to better visualise the breast tissue and/or abnormalities.
Health practitioners may recommend a breast MRI for women at higher-than-normal risk of breast cancer (i.e., those with genetic factors such as the BRCA 1 or 2 mutation), for women under 50 with dense breast tissue to further characterise a known abnormality on a mammogram/ultrasound or to look for cancer in the opposite breast when it has been found in one breast already.
Breast MRI is also used as a surveillance tool to look for recurrent tumours after previous breast cancer treatment, to gauge the body’s response to treatment such as chemotherapy, and prior to surgery to the breast or lymph glands.
How to perform self-examination keyboard_arrow_down
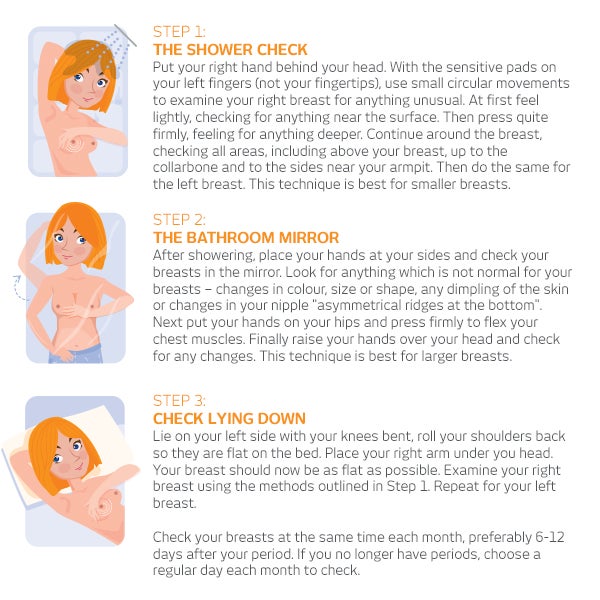
All women should check their breasts regularly between scheduled screenings - although it’s important to remember that self-checking is not a substitute for professional examination. If you notice any changes in your breasts, be sure to see your doctor.
3-step breast check
Spotting symptoms & risk factors of breast cancer keyboard_arrow_down
Educate yourself about breast cancer indicators and the factors that might elevate your risk. By understanding these elements, you're equipped to take swift, informed actions towards your well-being.
Breast cancer signs and symptoms
In the early stages of breast cancer there may be no symptoms at all. As the cancer grows, symptoms can include:
- A new lump or thickening in the breast, armpit area or around the collarbone.
- Change in breast size,shape or contour that is new or unusual.
- Changes to the nipple, such as rash, sores or crusting, an ulcer or inverted nipple.
- Clear or bloody (not milky) nipple discharge.
- Changes to the skin including redness, puckering or dimpling (an ‘orange peel/peau d'orange appearance).
- Breast tenderness or pain that does not go away.
- Swelling in part of the breast or the whole breast.
- Persistent itching or scaling on the nipple or areola.
It’s important to remember that most breast changes are not cancer, but any new or unusual symptom should be checked by a doctor promptly
Risk factors
A risk factor is something about a person, or what that person is exposed to, that increases their ‘risk’ (in other words, the chance or likelihood) of developing breast cancer in future. It can be genetic or due to a lifestyle factor like alcohol or lack of exercise. Importantly, risk factors don’t tell us everything and the existence of a risk factor, or several risk factors, does not mean a woman will be diagnosed with breast cancer.
Common risk factors include:
- Age (75% of women with breast cancer are aged 50+)
- Excessive alcohol consumption
- Family history/genetics
- Breast density
- Metabolic health
- Smoking
All women over age 50 should utilise the free services provided by BreastScreen Australia and schedule regular breast screening.
Types of breast cancer keyboard_arrow_down
Breast cancer occurs when abnormal or damaged cells grow in an uncontrolled manner and a tumour is formed. Most tumours start in the milk ducts which carry milk to the nipple. It can develop in both men and women, although it is much less common in men.
Breast cancer is not just one disease, but several. It includes different subtypes and treatments are becoming increasingly personalised for patients.
Non-invasive breast cancers (carcinoma in situ) are contained within the milk ducts or lobules in the breast and have not grown into the normal breast tissue:
- Ductal carcinoma in situ (DCIS) – a non-invasive breast cancer that is confined to the milk ducts of the breast.
- Lobular carcinoma in situ (LCIS) – a non-invasive breast cancer that is confined to the lobules or milk producing glands at the end of the milk ducts of the breast.
Invasive breast cancers are cancers that are growing in the normal breast tissue and have the potential to spread to other sites in the body:
- Early breast cancer – an invasive breast cancer that is contained in the breast and may or may not have spread to lymph nodes in the breast or armpit.
- Paget’s disease of the nipple – a rare form of breast cancer that affects the nipple and the area around the nipple (the areola). Commonly associated with invasive cancer elsewhere in the breast.
- Inflammatory breast cancer – a rare form of invasive breast cancer that affects the lymphatic vessels in the skin of the breast. This type of breast cancer does not present as a lump but rather a redness or rash in appearance.
- Locally advanced breast cancer – an invasive breast cancer that is large or has spread to areas near the breast, such as the chest wall.
- HER2-positive breast cancer – any type of breast cancer that tests positive for a protein called human epidermal growth factor receptor 2 (HER2).
- Triple negative breast cancer – breast cancer that tests negative for all three receptors – oestrogen, progesterone and HER2.
- Metastatic breast cancer – also known as advanced, secondary or stage 4 breast cancer, which has spread to other parts of the body such as the bones, liver or lungs.
The above information has been sourced from the Breast Cancer Trials website.
